
Ultimate Guide to Vein Treatments
Varicose veins and spider veins are unsightly and uncomfortable conditions that affect many people, and, in the case of varicose veins, they can lead to serious complications. To help alleviate the symptoms of varicose veins, you may consider laser or surgical procedures that are designed to relieve pressure on the veins and promote better circulation.
Fortunately, there are many different types of vein treatments to choose from, and they can all be performed on-site at a vein treatment clinic. The recovery time is minimal as well, so you’re able to return to your normal routine in no time.
If you’re considering vein treatment, take a look at this guide to vein conditions, vein treatments and what to expect before, during and after your surgery.
What Causes Varicose Veins and Spider Veins?
Though often regarded as a cosmetic issue, varicose veins and spider veins are symptoms of underlying vein problems. Left undiagnosed and untreated, varicose and spider veins can develop into other problems.
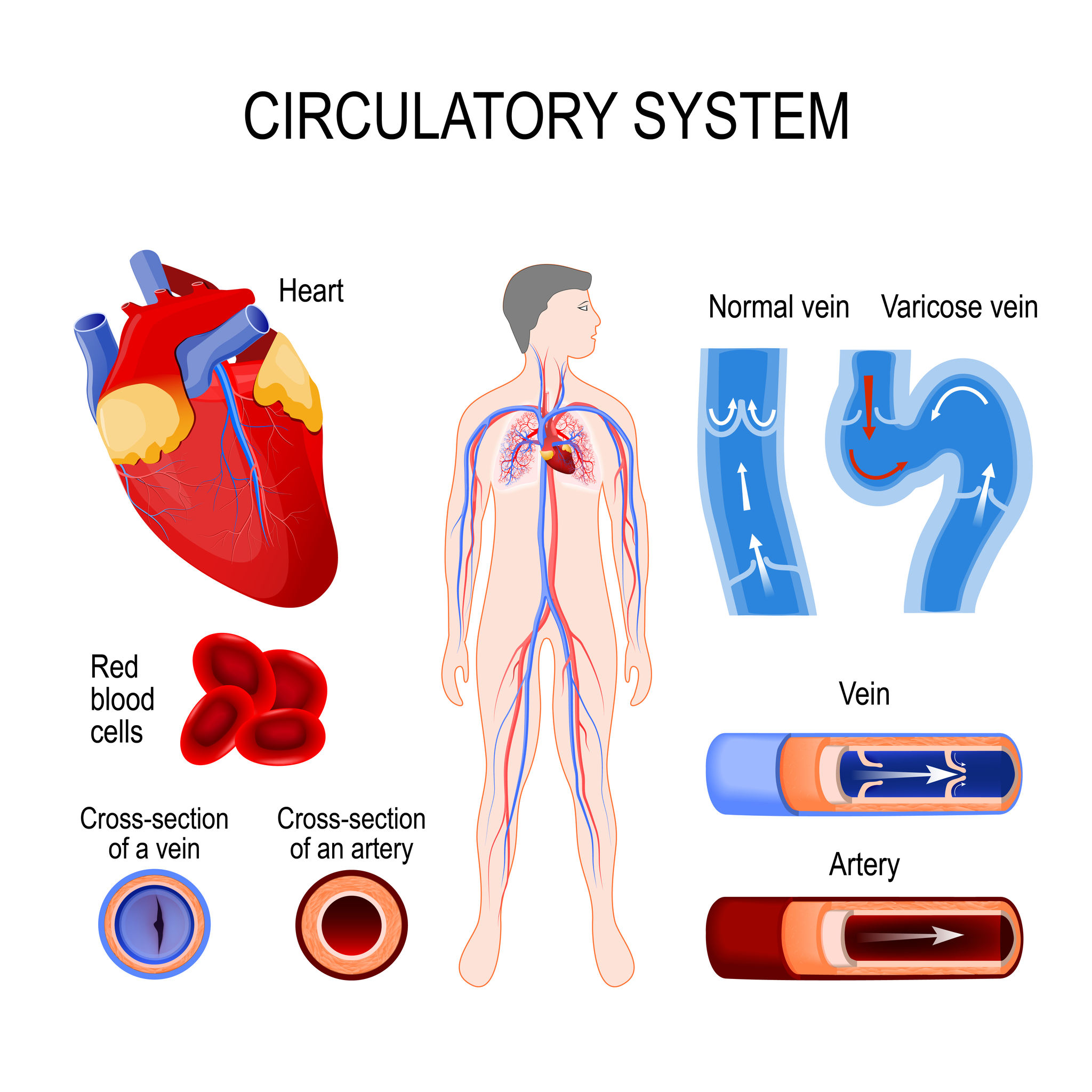
Both varicose veins and spider veins are symptomatic of an issue with your circulation. In healthy individuals, arteries transport oxygenated blood from your heart to your muscles, bones and tissues. When this oxygen is depleted, veins move the deoxygenated blood back to the heart, and it is then pumped back into the lungs for more oxygen. This process is challenging to your body, especially in the lower extremities, because your body needs to work against gravity to keep blood flowing properly.
Your veins also have a series of tiny back-pressure or flap valves that only open in one direction, ensuring that when normal, the blood flows back to your heart. If these valves are damaged by disease or injury, blood can flow backwards (reflux) and pool in the lower extremities, creating pressure and swelling in the veins. As this pressure builds, more valves can become damaged, along with the walls of your veins. With prolonged reflux, veins become weaker and more fragile, leading to a condition known as Chronic Venous Insufficiency, or CVI.
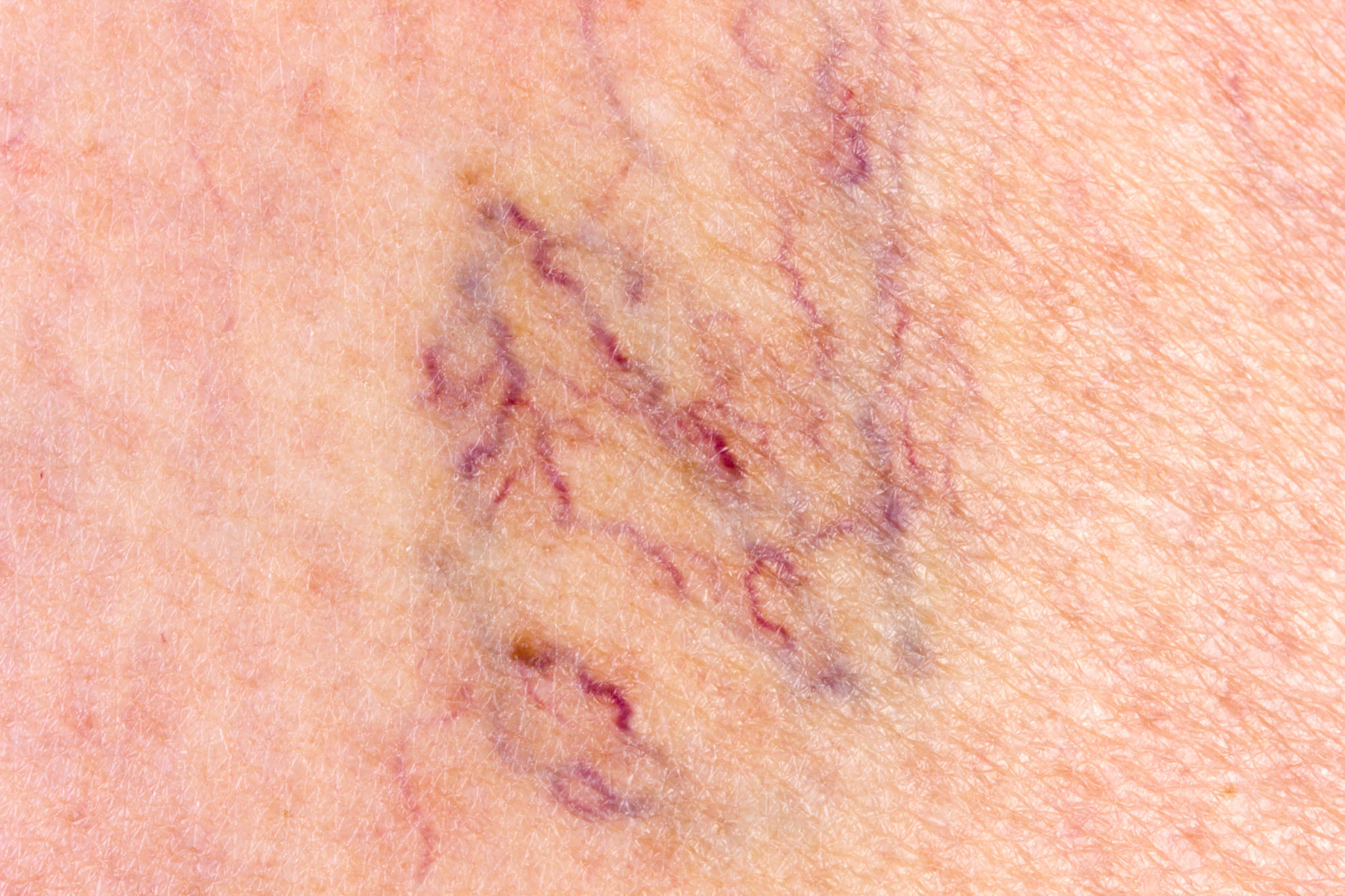
Varicose veins and spider veins occur when these issues affect veins close to the surface of the skin. With varicose veins, the veins protrude and may appear large and twisted, whereas spider veins look like a web of red, purple or blue lines.
What Are the Symptoms of Vein Disease?
Varicose veins and spider veins are visible symptoms of CVI, but they’re not the only symptoms. Many individuals with vein disease experience heaviness and weakness in the legs, or even sharp leg cramps that occur at night. As expected, restless leg syndrome is frequently connected to superficial venous reflux disease.
If left untreated, the swelling of leg veins can lead to many skin conditions, such as:
- Skin tightness.
- Skin itchiness.
- Discoloration in the legs and ankles.
- Fragile skin.
- Slow wound healing.
- Cellulitis, in extreme cases,
- Bleeding.
- Phlebitis.
- Deep Vein Thrombosis (DVT).
With prompt and accurate diagnosis, these symptoms can be relieved or prevented.
Conditions Related to Vein Disease
Unfortunately, the veins in your legs aren’t the only ones that may be affected by vein problems. Here are some other conditions related to vein disease:
- Hemorrhoids: Hemorrhoids are actually varicose veins that are found in or around the anus. These may cause itching, pain or bleeding, and are usually caused by bowel pressure. Fortunately, this condition can be easily treated with lifestyle changes. Surgery is rarely necessary.
- Leg ulcers: As venous disease advances, it may lead to painful ulcers that form on the skin near the varicose veins, mostly near the ankles. When the venous circulation is compromised, blood pools in the veins, also known as venous stasis, and increases pressure within affected veins. This causes skin breakage and ulcer formation, which require immediate medical attention.
- Sudden leg swelling: If you experience considerable swelling in your leg from enlarged deep veins, it’s important to see a doctor immediately. This may indicate thrombophlebitis, a painful condition in which a blood clot blocks a vein. On occasion, superficial venous thrombophlebitis may lead to a deep vein thrombosis.
Who’s at Risk for Vein Disease?
Vein disease usually affects individuals over the age of 50, but it may develop earlier for some. Certain risk factors for CVI are not always within our control, but they may be reduced through smart lifestyle choices.
There is a genetic component to vein disease as well, so if you have a family history of varicose and spider veins, you’re more likely to develop the condition. A history of blood clots, leg trauma or injury, or certain types of cancers may be all be factors as well, along with being a woman who is pregnant, has been pregnant, or is peri- or post-menopausal.

While these factors may be out of your control, you can still take preventative actions to lower your risk of vein disease. Avoid sitting or standing for long periods of time, maintain a healthy weight, stay active and avoid smoking or excessive drinking to reduce your risk of vein disease.
Self-Care for Vein Conditions
The best way to treat varicose and spider veins is by doing what you can to stay healthy and prevent them from forming. Here are some self-care tips to prevent or treat mild varicose veins:
- Avoiding standing or sitting for long periods of time. If it’s not possible to avoid prolonged sitting or standing, move your legs as much as possible to keep the blood circulating.
- Wear compression stockings to help your legs transport blood to the heart and prevent pooling of blood in the legs.
- Elevate your feet above your heart as much as possible.
- Engage in exercises that improve circulation in the legs, such as walking, jogging, running or swimming. This also helps you maintain a healthy weight.
- Try to eat healthier and lose weight if you’re overweight.
When Is the Best Time for Vein Treatment?
Vein disease affects about 25 million Americans. It can range from discomfort and heaviness in the legs with no visible signs, to spider veins, varicose veins, skin discoloration, skin thickening or skin ulcers. Generally, vein conditions start out small and worsen over time, but the future effects may be preventable with early treatment.
What Types of Vein Treatments Are Available?
Venous conditions can be treated with many different procedures, most of which are minimally invasive.

Here are the leading vein treatments:
- Venefit (VNUS Closure) Procedure: Radiofrequency Ablation (RFA): This is a non-surgical alternative for treating varicose veins. As an alternative to surgical stripping of the greater or lesser saphenous vein (and others), an RF probe is passed through an IV access. During this procedure, radiofrequency energy is used to heat and contract the collagen within the vein walls, causing the vein to collapse and seal. After it closes, blood is rerouted to healthy veins naturally. RFA is the gold standard against which other procedures are measured for comparison.
- Endoscopic Venous Laser Therapy. (EVLT). Many patients hear the word “laser” and envision its use as the most up to date or the least invasive or the least painful of procedures. This procedure is still commonly utilized. However over the years EVLT has been demonstrated to be less safe, less effective and more painful than Radiofrequency Ablation (RFA).
- Varithena Microfoam Chemical Ablation: This is a foam created by mixing polidocanol and oxygen. Although it is injected, it should not be confused with sclerotherapy. This injectable foam is used to treat certain refluxing veins and especially large and twisted varicose veins caused by problems with the greater saphenous vein and other related veins.
- Sclerotherapy: Sclerotherapy is performed with an injected chemical irritant that goes directly into the spider vein, shrinking it in size and relieving the associated discomfort.
- Asclera: Asclera is the most common sclerosing agent that is injected into the vein and damages the endothelium, or the cells lining the inside of the blood vessels. This causes platelets to attach to the lining of the vessels, causing the blood vessel to clot. Over time, the clotted vein will be replaced with scar tissue.
- Ambulatory Phlebectomy: Also known as stab phlebectomy. This procedure uses tiny punctures or incisions to remove the varicose veins.
- Vein Gogh Ohmic Therapy: This is a procedure that uses a tiny needle probe to deliver Radiofrequency and thermocoagulate and eliminate tiny blood vessels. It’s typically used to treat fine telangiectasias, broken capillaries, angiomas and spider veins that have shown resistance to other treatments. It’s also suitable for sensitive areas and areas of veins too small for injection of sclerosing agents such as Asclera.
- VenaSeal: This is a non-tumescent, non-thermal, non-sclerosant procedure that uses a proprietary medical adhesive delivered endovenously to seal off the vein.
Your vein doctor will work with you to determine the best vein treatment option(s) for your specific vein issues, medical history and desired results.
Vein Treatment Consultation
Before any decisions about your treatment are made, you’ll need to meet with the doctor for a consultation. This appointment will include a thorough discussion about your medical history, family history, vein conditions, vein symptoms and any previous injury or illness that may have resulted in vein damage. The consultation may also include an examination of your legs to check for swelling, and an ultrasound to examine the blood flow in your legs and identify any vein conditions.

The initial consultation is an excellent time to address any questions or concerns you may have. Be sure that you fully understand your treatment options and the risks and benefits involved, and that you feel completely comfortable with your treatment team. Bring a list of your current and past medications to your appointment, and be sure to disclose any medications you’re taking to be sure that they don’t impact your treatment.
You may also discuss your insurance coverage with the staff to see if your specific diagnosis and treatment are covered by your insurance and what, if anything you’ll be responsible for financially.
After vein ultrasound and mapping is completed, the physician can then complete your consultation. Specific treatment recommendations are then made. You will receive specific instructions for the time leading up to the day of the procedure as well as for immediately following the procedure. Be sure to follow these instructions carefully, and be sure you bring everything you need with you to the appointment.
The Day of the Procedure
On the day of the procedure, you’re free to eat or take any prescribed medications, unless you’ve been advised otherwise during your consultation. It’s advisable to wear loose-fitting clothing. At the conclusion of any procedure, you will have your leg firmly wrapped with compression bandages or you may be asked to wear your compression stockings.
Depending on the vein treatment will be made comfortable with a local anesthetic. Rarely is any sedative medication necessary. ANy sedative utilized is typically taken by the patient in pill form. If any sedative is taken, the patient will b e advised to arrange a ride home. Otherwise, typically, patients are comfortable and drive themselves home or back to work after a procedure.

At the start of any procedure, the treated leg will be sterilized and prepared for the planned procedure. During ablation and phlebectomy procedures, a local anesthetic will be injected along the course of the targeted vein or veins, then treated. With sclerotherapy procedures, the injections are placed directly into the targeted veins. Most vein procedures are completed in under an hour, depending on the size and number of veins treated and the treatment type.
Immediately after any procedure is completed, the treated area may be bandaged and/ or you’ll have a compression stocking placed on your leg. Compression stockings apply external pressure on your leg veins to reduce swelling and prevent blood from pooling in the veins, which helps with venous blood circulation. Compression stockings may also alleviate some of the discomfort following your vein treatment.
You’ll also have a printed copy of aftercare instructions and any prescribed medications to take home with you.
After the Procedure
After the doctor bandages your legs, you’re free to return home or to work. As mentioned, please arrange a ride if your treatment involves sedation.
Once you’re home, you’ll need to wear your compression wrap or stockings for the following two days without removing them. After that, you’re free to remove the stockings and bandages, and with most procedures, you’re able to get your legs wet. Your doctor will advise you if you need to avoid getting the treated areas wet, and for how long.
Most vein procedures are minimally invasive and carry few risks of complications, but it’s still best to take precautions to aid in recovery and minimize risks. Generally, you’re able to resume daily activities as soon as you return home, but you should avoid strenuous activity, heavy lifting or excessive stress for a few days, and wait at least one day to shower. It’s also important to avoid soaking in pools, hot tubs or bathtubs to minimize the risk of infection.
There’s usually only mild discomfort following vein treatments, but if you’re experiencing pain, the doctor may recommend ibuprofen (Motrin) or acetaminophen (Tylenol). If the pain continues or worsens, call your doctor, and make an appointment with your doctor for a checkup.
Side Effects and Complications
Most patients experience very minimal bruising, swelling, tightness and skin discoloration near the treated veins in the days following these procedures. These symptoms are not a cause for alarm. They typically may persist for a month but on occasion may persist for 3 months or more before compoletely subsiding. Numbness in the skin near treated veins may occur, but will usually dissipate over the same time.

During your recovery, you’ll have follow-up appointments with your doctor within the first month and once more after six months. Most often by 3 to 6 months after completion of all recommended treatments, any side effects should have dissipated, and you should be seeing the results of your vein treatment.
Visit Vegas Valley Vein Institute
In the past, there were few viable options for treating varicose veins and spider veins, and what was available was highly invasive. Surgery was debilitating, requiring prolonged periods of lost work. Fortunately, recent advancements in the treatment of varicose veins, spider veins and other vascular conditions have made it possible to remove unsightly and uncomfortable veins with effective, minimally invasive procedures that provide permanent results. Many health insurance providers cover vein treatments as well, making them more accessible than ever.
If you’re considering vein treatment for your varicose veins, spider veins or other vascular conditions, Vegas Valley Vein Institute would love to help. We combine the best of traditional methods and state-of-the-art, non-surgical treatments to provide you with the ideal vein treatment customized to your needs and to give you results that last. Contact us today to learn more about our vein treatments!