Deep Vein Thrombosis
Deep vein thrombosis (DVT) happens when a thrombus, or blood clot, occurs in one or more of the deep veins in your body. While a DVT can form in other areas, they most commonly occur in the legs.
Though DVT typically causes leg pain or swelling, instances may also occur without symptoms, making them much harder to detect. DVT usually develops as the result of medical conditions that affect the way the blood clots or as a result of sitting for extended periods of time.
Left untreated, a DVT blood clot can break off and travel to the lungs, causing a pulmonary embolism, which is life-threatening. It can also lead to complications in the legs, such as post-thrombotic syndrome and chronic venous insufficiency.
Fortunately, a DVT is preventable, and it is treatable if discovered early.
Description and Symptoms of Deep Vein Thrombosis
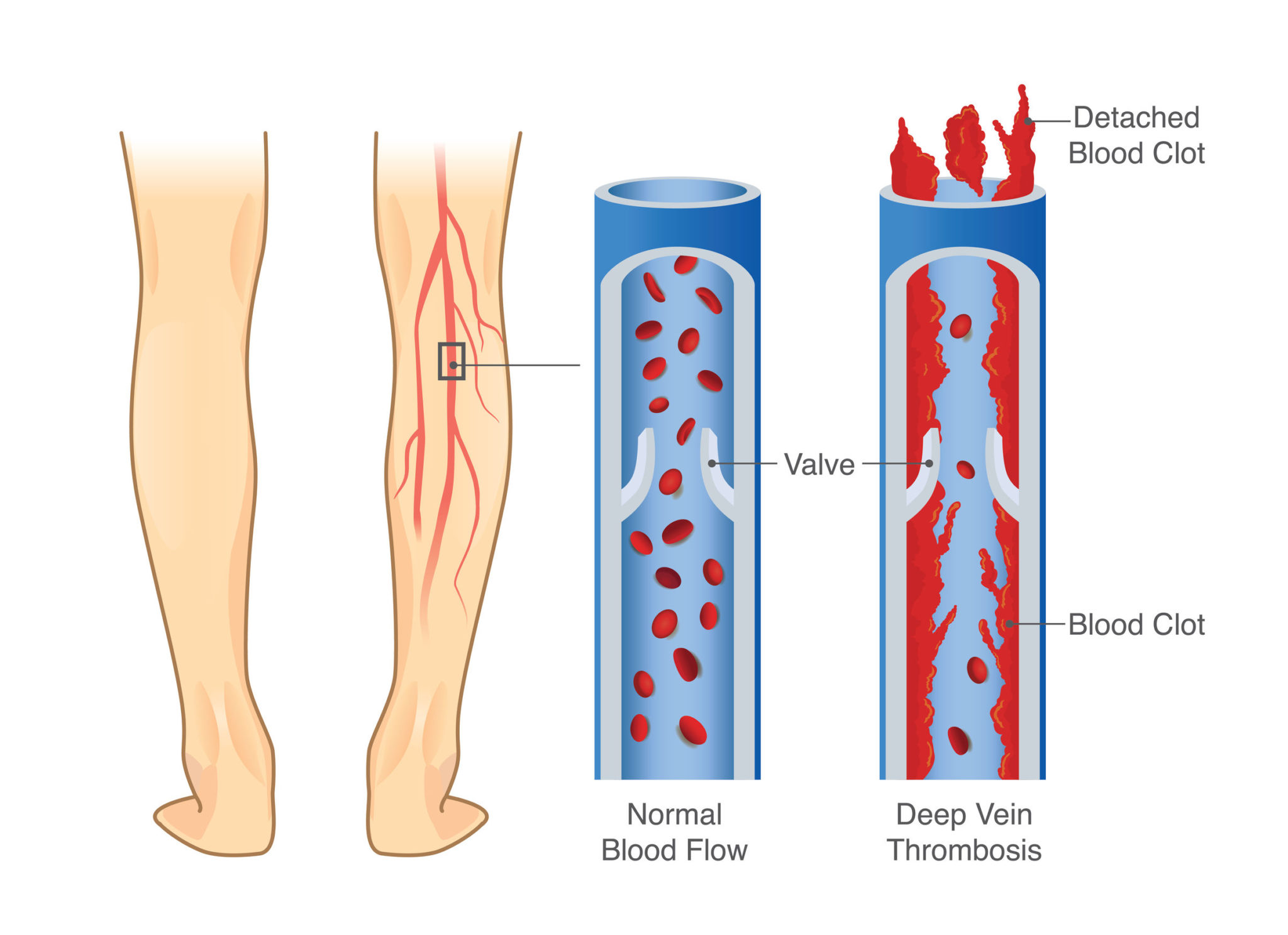
The circulatory system contains both arteries and veins. Arteries carry oxygen-rich blood from the heart to other tissues in the body, while veins return the oxygen-depleted blood back to the heart.
There are two types of veins:
- Superficial veins, which lie just below the surface of the skin.
- Deep veins, which are located deeper, within the muscles.
In most cases, a DVT only forms in one leg or one arm, rather than both. The symptoms of a DVT may include:
- Swelling of the affected leg or arm, which may occur suddenly.
- Pain or tenderness in the affected leg or arm, which may only occur when walking or standing.
- Warmth in the affected area.
- Red or discolored skin in the affected area.Though this should NOT be confused with signs of a superficial venous thrombosis.
- Enlarged veins near the skin’s surface in the affected area.
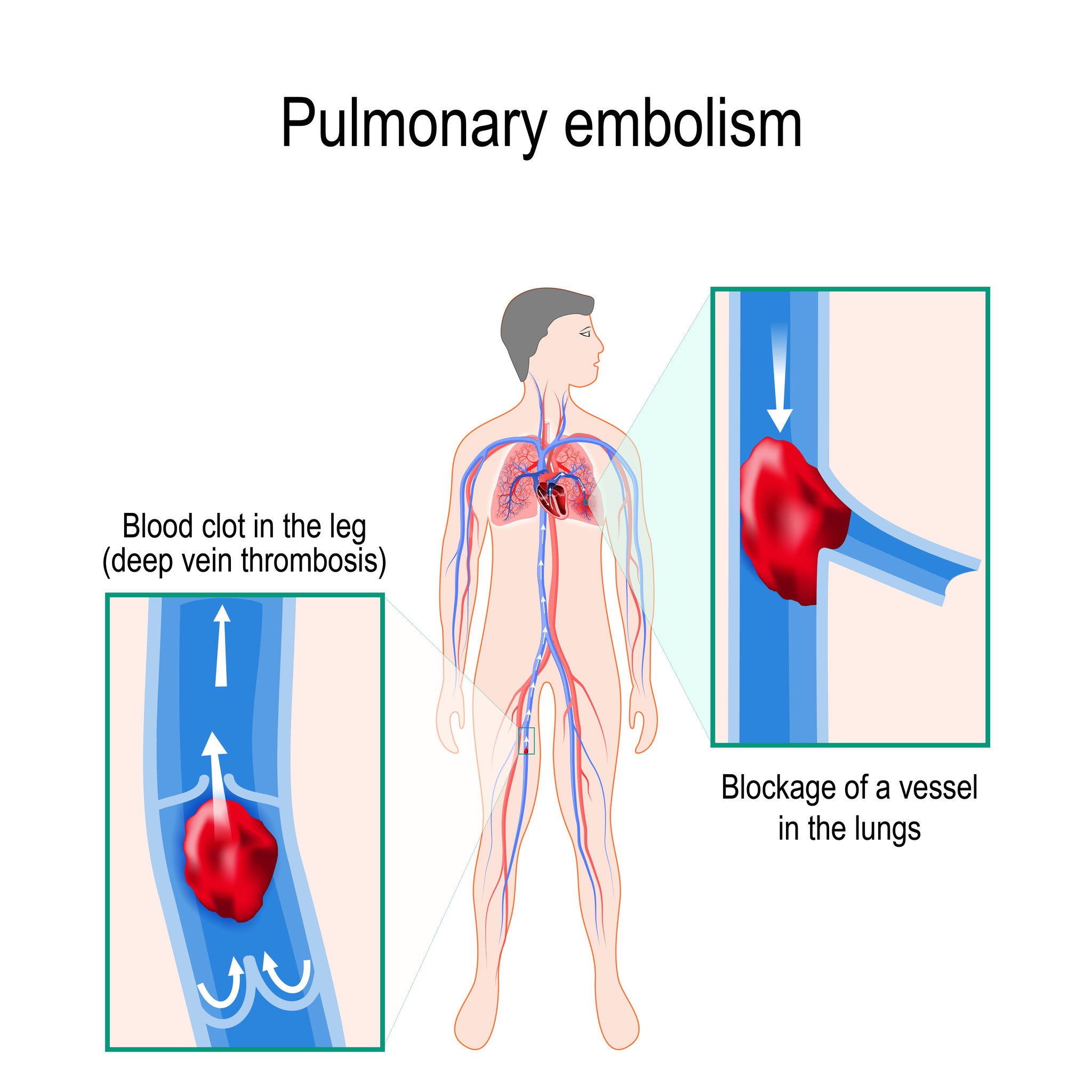
If the DVT dislodges or breaks off and traveled to the lungs, causing a pulmonary embolism, the symptoms may include:
- Sudden shortness of breath or rapid breathing.
- Sharp chest pain that is worsened by coughing or movement.
- Back pain.
- Cough, with or without bloody sputum or phlegm.
- Excessive sweating.
- Rapid heartbeat.
- Dizziness or fainting.
In some cases, patients are unaware of a DVT until the clot moves to their lungs. Because of this, it’s important to seek medical attention if you notice any symptoms of a DVT or pulmonary embolism, to prevent serious complications.
Difference Between DVT and Superficial Venous Thrombosis
A superficial venous thrombosis, also called superficial thrombophlebitis or phlebitis, is a blood clot that develops in a superficial vein. These types of blood clots are unlikely to travel to the lungs or cause life-threatening complications, unless they move from the superficial vein to the deep venous system. This is a rare occurence.
Risk Factors for DVT

A DVT can occur in anyone, regardless of age, race, activity level, or prior medical conditions. Certain factors can increase the chance of developing a DVT, however, especially if several occur at the same time.
Here are some factors that increase the likelihood of developing a DVT:
- Injury to a vein, which may be caused by fractures, significant muscle injury, or major surgery of the pelvis, abdomen, hip, or legs.
- Slow blood flow, which may be caused by confinement to bed, limited movement, sitting for long periods of time, or paralysis.
- Excess estrogen, which may be caused by birth control pills, hormone replacement therapy, or pregnancy and post-pregnancy.
Certain chronic medical conditions can increase the risk as well, such as:
- Heart disease.
- Lung disease.
- Cancer.
- Cancer treatment.
- Inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease.
Other risk factors may include:
- Previous instances of DVT or pulmonary embolism.
- Family history of DVT and pulmonary embolism.
- Obesity.
- Age.
- A catheter within a central vein.
- Genetic clotting disorders.
Complications of DVT

The most serious complication of DVT is when the clot breaks off and travels to the lungs, resulting in a pulmonary embolism. Like DVT, a small pulmonary embolism that’s treated quickly and effectively can end in a full recovery, but there is a risk of lung damage or death. A massive DVT can be fatal within minutes.
DVT can also result in long-term complications from the damage that occurs to the valves in the veins, which is called post-thrombotic syndrome. Patients with post-thrombotic syndrome develop symptoms like pain, aching, and itching in the legs, skin discoloration, swelling, and in severe cases, scaling or ulceration in the affected area. These symptoms can be severe enough to cause disability.
Chronic venous insufficiency is another long-term complication of DVT. This is a condition in which the venous walls or valves in the vein are no longer working effectively, making it difficult for the blood to return to the heart from the legs. This causes blood to collect in the veins, known as stasis. The symptoms of chronic venous insufficiency include swelling, aching, and weakness in the legs, leathery skin, flaking or itching in the skin, venous stasis ulcers, and varicose veins.
Despite a widely held belief, a DVT does not cause a heart attack or stroke. These are caused by the blockage of an artery, known as arterial thrombosis. These types of clots can be serious, since they can obstruct the flow of blood to major organs, such as the heart or brain, leading to heart attack or stroke.
In addition, a DVT or pulmonary embolism can become chronic, with roughly 30 percent of patients at risk for recurrence.
DVT Prevention

Like most medical conditions, DVT and pulmonary embolisms are much easier to prevent than treat.
Here are a few preventative measures to lower your risk of DVT:
- Stay mobile, especially after bed confinement, such as after an injury, illness, or surgery. Be as mobile as possible, directed by your doctor.
- Wear loose-fitting clothing. More important, do not wear tight clothing that restricts the blood flow in your leg veins.
- When sitting for long periods of time, try to walk every hour, certainly every two or three hours. Exercise your legs by raising and lowering your heels and toes or by contracting and releasing the muscles of your legs.
- Use graduated compression stockings, as directed by your doctor.
- Talk to your doctor about medications to prevent DVT.
- Avoid a sedentary lifestyle.
- Maintain a healthy weight.
If you’re concerned about developing DVT or a pulmonary embolism, speak with your doctor about specific preventative measures that are appropriate for your current health conditions and family history.
Diagnosing DVT

If DVT is suspected, a doctor will perform a thorough exam and review your medical history to look for risk factors. Several tests are administered to diagnose a DVT, such as:
- Duplex venous ultrasound: This is a common diagnostic test for DVT. A duplex venous ultrasound shows blood flow in the veins and detects any existing blood clots. The ultrasound technician will apply pressure to the leg or arm, and if the vein doesn’t compress, it could indicate the presence of a blood clot.
- Contrast venography: This test uses an x-ray to show the deep veins by using contrast material injected in the vein. Abnormalities, blood clots, or blockages are then visible. This testing may be used if the duplex venous ultrasound results are inconclusive.
- Magnetic Resonance Imaging (MRI) or Magnetic Resonance Venography (MRV): An MRI shows organs and structures within the body, and an MRV shows the veins. These two types of imaging can provide a more comprehensive picture than an x-ray.
- Computed Tomography (CT) scan: This is a type of x-ray that shows the structures within the body. A CT scan may be used to detect a DVT in the abdomen or pelvis, as well as to detect a pulmonary embolism.
If a genetic component is suspected, blood tests may be needed, such as the D-dimer blood test, which measures a substance in the blood that’s released when the clot breaks up. This is important if:
- You have a history of blood clots that don’t have an apparent cause.
- You have a blood clot in an unusual location, such as the veins in the liver, kidney, brain, or intestines.
- You have a family medical history of blood clots or clotting disorders.
Treating DVT

Patients with DVT may need hospitalization, though less severe cases may be treated on an outpatient basis. The goals of treatment are as follows:
- Stopping the clot from getting bigger.
- Preventing the clot from breaking off and traveling to the lungs, leading to a pulmonary embolism.
- Reducing the risk of developing recurrent clots.
- Minimizing the risk of developing serious complications.
Common treatments include:
Anticoagulants
These are “blood thinning” medications that affect the blood’s ability to clot. Though these medications are called “blood thinners,” they don’t actually thin the blood. Instead, they reduce the ability of the blood to clot. Anticoagulants can stop clots from getting bigger or moving to other areas of the body as well.
Anticoagulants don’t dissolve or destroy a clot, but the body has the natural ability to resorb it. In some cases, a clot will be dissolved by the body, but won’t disappear entirely.
The most common injectable anticoagulants are:
- Unfractionated heparin injected intravenously (into the vein).
- Low-molecular-weight heparin injected subcutaneously (under the skin).
- Fondaparinux injected subcutaneously.
The most common oral anticoagulants are:
- Warfarin.
- Dabigatran.
- Rivaroxaban.
- Apixaban.
- Edoxaban.
Anticoagulants may only be prescribed for three to six months, but may be prescribed for longer periods in patients with:
- Recurrent DVT or pulmonary embolisms.
- Presence of other chronic conditions, such as cancer, that may increase the risk of a blood clot.
Different anticoagulants have different side effects, but the most common are bleeding, such as nosebleeds or bleeding gums, and bruising. In these cases, it’s best to consult a doctor to avoid any serious complications.
Thrombolytics
Thrombolytics are medications that actually act to dissolve blood clots to improve blood flow and prevent damage to the tissues. While these are effective medications for dissolving clots and preventing complications, they do carry a higher risk of excessive bleeding, so they are only used in severe cases.
Inferior Vena Cava Filter
If anticoagulants aren’t appropriate for treating DVT, a filter may be inserted within the inferior vena cava, a large vein that carries deoxygenated blood from the lower body to the heart, to remove or trap a clot before it reaches the lungs.
Thrombectomy
In severe cases, a thrombectomy may be used to remove the clot and prevent it from causing serious complications. This is a surgical procedure that involves an incision in a vein to remove the clot, then repairing the venous wall to restore blood flow. In some cases, a balloon-like device is used within the vein to prevent collapse.
If the clot is near the lungs, an embolectomy may be appropriate. This is a surgical procedure that involves an incision or a catheter inserted in the affected vein to remove the clot.
These procedures are usually recommended in emergency situations where other clinical interventions are not effective.
Compression Stockings
Graduated compression stockings, also called medical compression stockings, may be used to prevent or reduce leg swelling. Swelling often occurs as a result of damaged valves within the leg veins. Most compression stockings are worn to just below the knee and are tight throughout the ankle, gradually loosening as they reach the knee. This provides consistent, gentle pressure on the leg. However, thigh high or pantyhose high compression stockings are often more appropriate and effective .
Preparing for Your Appointment

A DVT is considered a medical emergency, so it’s vital to seek medical attention immediately if you suspect one. If there’s enough time, however, there are a few things you can gather to help your diagnosis and treatment.
Make a list of:
- Your symptoms, including any that seem unrelated but that may have appeared suddenly, and when your symptoms began.
- Family history of blood-clotting disorders.
- Your medical history, including hospitalizations, surgeries, traumas, or chronic illnesses.
- All medications you take, including vitamins or supplements, and their dosages.
- Questions you may want to ask.
Some questions you may want to ask include:
- What’s the most likely cause of the symptoms?
- What diagnostic testing can be expected?
- What type of treatment is available?
- What alternative treatments are available?
- Are there any restrictions on physical activity or travel?
- What’s the best way to manage DVT and existing medical conditions?
- Are there any recommended printed materials or resources for DVT?
You should also expect questions from your doctor, such as:
- Have you been inactive lately, such as lying down or sitting for long periods?
- Are your symptoms constant, or intermittent?
- Are your symptoms more or less severe at different times, such as early morning or after exercising?
- Does anything improve your symptoms?
- Does anything worsen your symptoms?
The more information you can provide to your doctor, the more effective and prompt your diagnosis and treatment can be.
Varicose Veins and DVT
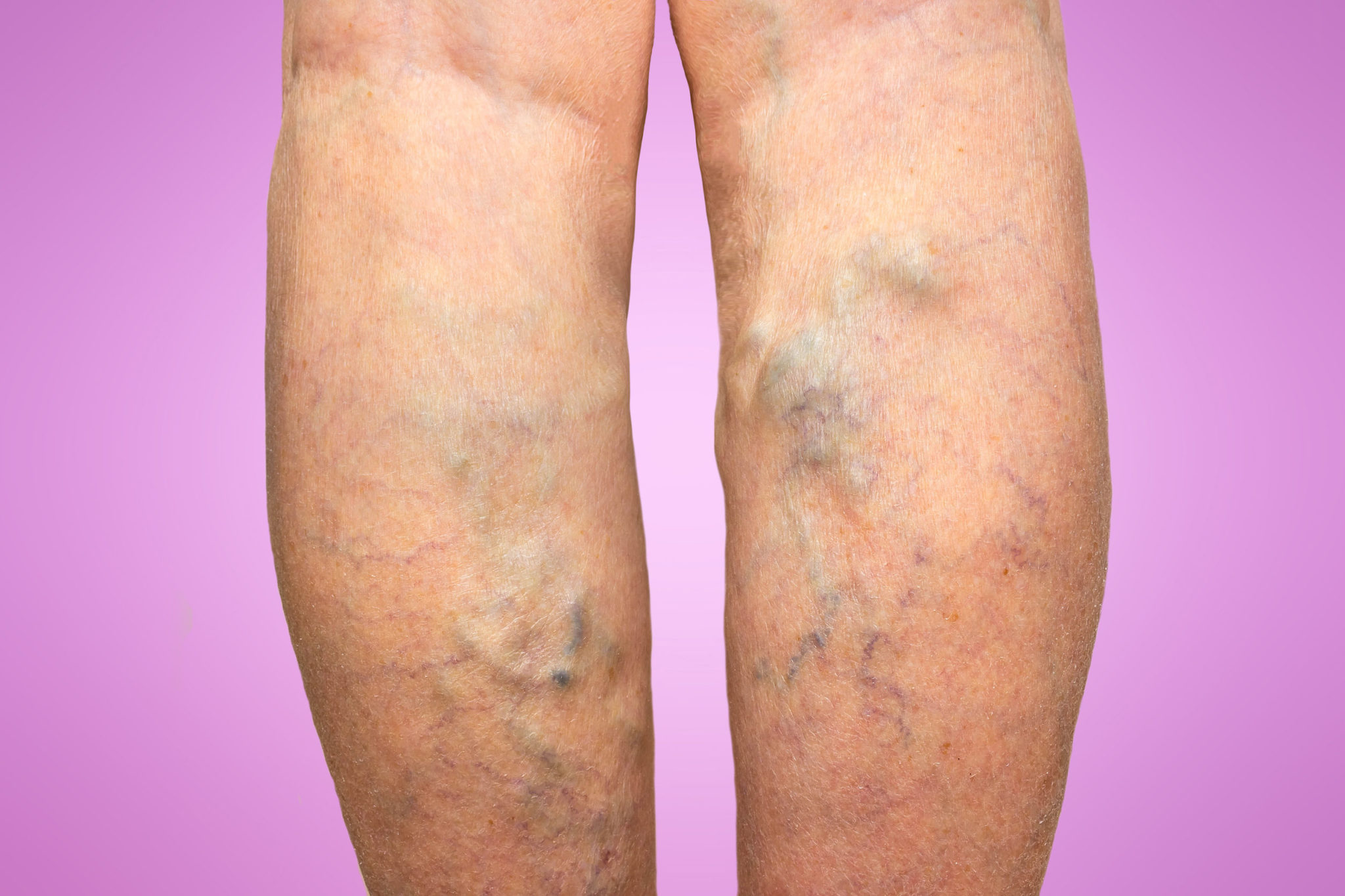
According to a study in the Journal of the American Medical Association (JAMA), there’s a significant association between varicose veins and DVT, with less significant associations with pulmonary embolisms and peripheral artery disease.
The finding of this retrospective study of over 400,000 people is that varicose veins are a common condition, but they can be associated with more serious health risks, such as DVT and other vascular conditions. Varicose veins (Superficial veins) do not typically cause DVT. Rather it is the other way around. Further research is needed to determine if there is a causal relationship between varicose veins and DVT, as well as if there’s a common cause of the two, but it could indicate the importance of early evaluation of varicose vein disease.
Varicose veins are veins that become twisted and enlarged, most commonly in the legs, which can result from weak or damaged valves. Healthy veins return deoxygenated blood back to your heart, working against gravity to travel through tiny valves that, when working properly, stop the blood from flowing backward. If these valves are weak or damaged, blood can pool in the vein, causing it to stretch or twist.
In addition to being uncomfortable and unsightly, varicose veins can be painful and carry a risk of chronic swelling and venous stasis ulcers, which are open wounds that are difficult to heal. Varicose veins may also progress to a condition known as stasis dermatitis, which is a red rash on the skin in the affected area that may become shiny, hairless, and discolored. Venous stasis dermatitis is alate complication of superficial venous reflux and varicose veins, often progressing to painful open sores (leg ulcers).
In most cases, varicose veins only worsen with time, so early treatment is recommended to prevent complications like pain, cramping, itching, swelling, and fatigue.
Visit Vegas Valley Vein
Though many patients with varicose veins have a problem localized to the leg, there are hereditary and medical factors that can cause or worsen varicose veins and their associated complications, such as DVT.
If you are suffering from varicose veins, it’s important to seek evaluation and treatment from a vein specialist, such as Dr. Simon at Vegas Valley Vein. After evaluating your medical history and the severity of your condition, we’ll recommend the appropriate testing and vein treatment for your needs to help you relieve the suffering of varicose veins. Contact us today to schedule your consultation!